- Information for Adults Attending Heart Clinics
The purpose of this information
-
Who this information is for
- 2024-12-27
Date Published
Information for Percutaneous Pulmonary Valve Implantation
Contents
What is a percutaneous pulmonary valve implantation procedure?
What information will I be given to help me decide?
What happens before the procedure?
What happens on the day of the procedure?
What happens after the procedure?
What problems might happen during or after the procedure?
How do I look after myself when I go home?
Who can I contact for more information?
You have recently been informed that you have a problem with one of the valves in your heart called the pulmonary valve. The pulmonary valve is located on the right side of your heart between the right sided pumping chamber and the main lung artery. We understand that you may be worried about what this means for you. The information below will answer any questions you may have about the procedure and your hospital stay.
What is a percutaneous pulmonary valve implantation procedure?
A percutaneous pulmonary valve implant involves using a keyhole procedure to replace the pulmonary valve which is damaged. A small catheter (a small tube) will be inserted in your groin, neck or chest. This small tube is used to insert the new valve. This procedure is performed under a general anaesthetic (whilst you are asleep), by a team of heart doctors who are trained to perform keyhole procedures in people with congenital heart disease.
Sometimes a trans-oesophageal echocardiogram (T.O.E) is performed at the same time. A tube is passed down the back of the throat into the oesophagus (food pipe). This allows the doctor to get clear pictures of your heart from a different angle and is helpful in providing a more detailed picture of your heart.
During the procedure the doctor will move the catheter to measure the pressures in different parts of the heart and blood vessels. A contrast dye is injected through the catheter so that X-rays can be taken to help the doctors see the heart and blood vessels in more detail.
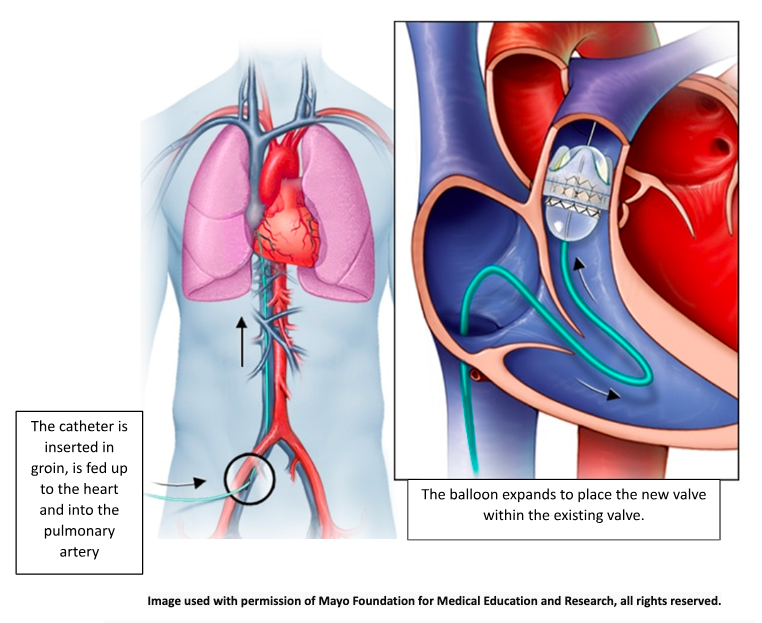
A large vein in the groin, neck or a small incision in the chest is used to enter the pulmonary artery. The new valve is implanted inside a wire mesh tube called a stent before carefully placing it into position with the use of a small balloon.
What information will I be given to help me decide?
You will be invited to clinic to talk to one of the heart doctors about your procedure. They will explain the reason why your heart valve needs replacing and how the procedure is going to be performed. They will discuss with you the small chance of any problems happening during or immediately after the procedure. These are called risks.
If you would like to understand more about the risks and benefits, you can read the NICE Guidance for patients here:
What will happen before I have my procedure?
We advise all patients to attend their dentist if they haven’t had a dental check in the previous 6 months. It is important to make this appointment as soon as you are told that you need a heart procedure. Tell your dentist that you need a procedure on your heart. Any dental work must be completed before you can have your procedure to prevent the risk of infection.
Problems with your teeth or gums can allow bacteria (bugs) to enter your bloodstream. People who have an existing heart condition have a higher risk of developing a condition called endocarditis. This is an infection affecting the inside of your heart and it can damage heart valves. It is often very difficult to treat and can be dangerous. After you have had your new valve inserted it is important to continue to look after your teeth. It is recommended that you continue to visit your dentist every six months for the rest of your life.
You will be invited to attend a pre-admission clinic. You will meet one of the congenital heart nurse specialists who will explain everything. You will be able to discuss your procedure in more detail and they will answer any questions you or your family may have.
At this appointment you may have the following tests:
- ECG (a trace of your heart rhythm)
- Some people may require an echocardiogram (heart scan)
- Blood tests
- Swabs to check for infection
Please bring all your medicines to the pre-admission clinic. You will be advised of any medications that need to be stopped prior to your procedure and when to stop taking them.
We advise you take all other morning medications as usual with a sip of water on the day of your procedure before 7am.
- Aspirin or Clopidogrel
It is important that you take these medications as normal. Please do not stop taking these.
- Blood thinning medication
You will need to stop taking your blood thinning medication prior to your catheter procedure. Anti-coagulation may be managed in various ways. The congenital heart nurse specialist will tell you exactly what you need to do depending on the medication that you take.
- Diabetic medication
You will be given specific instructions about your diabetic medication. Please do not take Metformin on the morning of your procedure as this will interfere with the dye used during the procedure. Other diabetic medications need individual care to ensure your blood sugars stay controlled.
The procedure is performed using X-rays which can be harmful to an unborn baby. It is important to check that you are not pregnant. Any person of childbearing age will be asked when their last menstrual period was. If it is greater than 28 days or you cannot remember, you will be asked to take a pregnancy test. This is normally checked with a urine test. We will need to wait for the results before you can have your procedure. If possible, try to keep a note of when you had your last period as soon as you know that you are going to have your procedure. Bringing this information with you may help to prevent a delay to your procedure on the day.
The congenital heart nurse specialists can provide additional support for anyone with special needs or learning disabilities. They will work closely with the patient and family or carers. This may include the following:
- Provide easy read information about the procedure
- Refer you to the hospital Learning Disability Liaison team if available
- Refer to a local learning disability team for extra help and support
- Provide a learning disability passport all about you and will make sure it is available for the staff
- Assess whether the person having the procedure can make the decision for themselves. This is called having capacity to consent.
- If the person doesn’t have capacity to make the decision for themselves the congenital heart nurse specialist will coordinate a best interest meeting
- Make sure that parents, family, or carers are fully involved and that any adjustments that are needed are put in place. This may include special arrangements for family or carers to be available to help support the person during the day.
What happens on the day of the procedure?
The timing of your admission will be confirmed when you are given the date of admission. It is possible that this date may change if unplanned emergencies occur. We understand that it can be very difficult for things to change at short notice. Please call the congenital heart nurse specialists for more information if this happens.
You will be admitted to the ward on the evening before or on the morning of your procedure:
- One of the nursing staff will check all your details again to make sure nothing has changed.
- A cannula (a small plastic tube) will be inserted into your arm or hand. This will be used to give fluids and drugs before, during and after your procedure.
- The nurses will place an identity bracelet on your wrist.
- Close to the time of your procedure you will be asked to change into a gown or pyjamas. You will also be given paper underwear to wear.
- The nurses on the ward will go through your consent form with you once again and will ask if you are still happy to go ahead with the procedure. If you have any last-minute questions don’t hesitate to ask.
- The nursing staff can organise for one of the doctors or the congenital heart nurse specialists involved in your care to come see you and answer any questions.
- The anaesthetist (the doctor who looks after you whilst you are asleep) may come and see you before your procedure.
- You will be taken into the room where the procedure will take place. It looks like an operating theatre. This is where you will be introduced to the team who will be looking after you during your procedure.
- They will once again check your details with you and the procedure that is being planned. They will perform a final safety check by running through what is expected to happen. You will be able to hear them make these checks.
- You will be able to stay with your child until they are asleep.
Picture of where the procedure will take place

What happens after the procedure?
- You will be taken to the recovery area after your procedure.
- Parents/ cares will be able to be with their child as soon as they are awake.
- When you feel more awake you will be transferred back to the ward area on a bed.
- You will be monitored very closely for several hours after your procedure.
- They will check your blood pressure and oxygen levels regularly.
- You will have a heart scan called an echocardiogram after your procedure.
- The will monitor your groin for any signs of bleeding.
- You will need to stay flat immediately after your procedure to ensure that the blood vessels have time to heal.
- The nursing staff will advise you when you can begin to sit up and walk around.
- You will still have the cannula (small plastic tube) in your arm after the procedure.
- Once you have woken up you will be offered something to eat and drink. You will be able to have the cannula taken out after this.
- The doctor will come to see you on the ward and will tell you all about your procedure. If you are not able to remember what was said or need help understanding the information, you can call the congenital heart nurse specialists who will chat to you about the results or organise for you to come back to clinic to speak to one of the doctors.
- You will normally be able to go home the day after your procedure.
- Pressing on the site usually stops any bleeding.
- Following your procedure, the blood vessel may have been sealed by a closure device called an Angio-seal, ProStyle or similar. This closes the hole in the artery or vein and reduces the risk of bleeding and the amount of time you must remain on bed rest. If you have had an angio-seal. The device is absorbed naturally within 60 to 90 days. You will be given instructions on how to care for this before you go home.
- Sometimes a special device is used to stop the bleeding just after the procedure. This device is attached to a belt and applies direct pressure to your groin. This may feel uncomfortable when fitted and will restrict your ability to move.
- If the bleed has been very large you may require some iron medication to help treat any anaemia.
- You may be bruised and tender following the procedure if bleeding occurs.
You may need a blood thinning drug (heparin) to be given via an intravenous infusion (drip). If this fails to work then a clot busting drug (alteplase) is given, again through a drip. It may delay your discharge home by a few days.
This is quite rare as you will receive a blood thinning drug during the procedure to prevent blood clots forming. However, clots can still form. If a clot develops, there is a small risk it can travel to the brain. The effects usually last only for a short period of time but very rarely a permanent stroke can occur.
(heartbeat which is too fast or too slow). Sometimes the heart can beat abnormally while the catheter moves inside the heart. Usually, it returns to normal once the procedure is over, but occasionally, medications, an electric shock or a temporary pacemaker may be needed to stabilise the rhythm.
This is rare and usually no action is required. Sometimes a needle will be used to remove blood from around the heart and rarely an open-heart operation is needed to repair the damage.
Occasionally it may not be possible to implant the valve during the procedure. The doctor will explain what this means for you and if there is a chance this might happen. They will also discuss what other options may be available to you if this were to happen.
Some of these risks may be increased further in the following situations:
– If you have pre-existing high blood pressure in your lungs
– If you have a pre-existing bleeding or clotting disorder
– If you have a heart condition where your lips and nails are cyanosed (blue)
– If the pumping action of your heart is not as good as it should be
You can ask the doctors for more information to help you understand all the above.
How do I look after myself when I get home?
The nurses on the ward will give you written information and explain any instructions prior to going home. Please remember to ask any questions before you leave.
- There may be bruising around the puncture site which is to be expected. If there has been some bleeding, then the affected area may be quite large. The bruising can develop over the next few days.
- A small dressing will be put on to the puncture site and we advise that it remains covered for at least 24 hours.
- The ward staff will provide you with some dressings to take home.
- You can have a shower the day after the procedure.
- Gently pat the wound dry and reapply the dressing.
- We advise you avoid having a bath for several days after the procedure and recommend you avoid applying any soap, talc, or creams onto the puncture site until it has fully healed.
- Approximately 1 week after the procedure you may notice a hard pea sized lump develop at the puncture site. This is quite common, not a cause for concern and it will eventually disappear
- You may experience some pain or discomfort for up to a week after the procedure particularly if you have a bruise
- Loose fitting clothing may help ease the discomfort around the puncture site
- You can take paracetamol if needed – but do not exceed the recommended dose
- You may feel tired for a day or so after the procedure. We recommend you rest for the remainder of the day when you go home. If you have had the test done through the top of your leg, try to limit the number of times you use the stairs to just a couple of times during the first 24 hours.
- You must not drive for 48 hours after a general anaesthetic. It will depend on how long it takes for any bruising to settle in your groin area before you can drive again. You must not drive until your groin feels normal and is no longer painful.
- You must tell DVLA if you have congenital heart disease and have symptoms that affect safe driving (for example angina, palpitations, shortness of breath, or symptoms related to high blood pressure, heart failure or heart valve disease).
- You can visit the DVLA website for specific advice at Congenital heart disease and driving
- You should avoid cycling or other sporting activities for at least a week or until your groin has fully healed and is no longer painful. You should be able to resume normal activities after this. Activities that increase your cardiovascular fitness are helpful and beneficial. You should avoid isometric static exercises such as heavy weightlifting where you must hold your breath and strain to lift. Please speak to the congenital heart nurse specialists if you would like individual advice about returning to contact or competitive sports.
When to contact the Team for advice
It is very important to contact the congenital heart team at either Alder Hey or Liverpool Heart and Chest hospital as soon as possible (link to contact page) if any of the following occur. If in any doubt, and you are worried please call NHS 111 or in an emergency attend A+E or dial 999
– If the wound site becomes red, swollen, or painful or is weeping
– You feel ‘pins and needles’ in the leg
– The leg becomes discoloured, appears swollen or feels colder than the other leg
– You become breathless or there is a change in your normal colour
– You become very sleepy or develop a high temperature
– It would be unusual for bleeding to occur once you are at home. However, if this happens you should lie down and apply firm pressure just above the puncture site for 15 minutes. If the bleeding does not stop after this time, you should contact your GP, NHS 111 or local Accident and Emergency department.
Who can I contact for more information?
This procedure is only performed at either Alder Hey Children’s Hospital or Liverpool Heart and Chest Hosiptal. If you have any worries or concerns, you can contact the following staff:
Congenital heart nurse specialists: 0151 252 5291
(You can call and leave a message 24hrs a day. The messages are picked up between Monday-Friday 09.00 am - 4.00 pm)
For Urgent queries outside of normal working hours:
Contact Alder Hey Children’s Hospital Switch Board on 0151 228 4811 and ask to be put through to Ward 1C for advice.
Congenital Heart Nurse Specialists: 0151 254 3333
(You can call and leave a message 24hrs a day. The messages are picked up between Monday-Friday 08.00 am - 6.00 pm)
Birch Ward: 0151 600 1175/1230
Hospital switchboard: 0151 600 1616